Hidden Heroes In Healthcare
Exploring the emerging layer of subclinical human capital that is driving better health outcomes
Every month we write a piece encompassing themes within our whole-person health investment thesis. If you would like to receive it directly in your inbox, subscribe now.
For this month’s edition, we are featuring a guest post from NEXT VENTŪRES investor, Jordan Pascasio. Given last month’s coverage of social determinants of health (SDoH) data, we wanted to take a deeper dive into the social-first care services that are driving greater accessibility for high-risk and at-risk populations.
There has been a noticeable wave of companies across the entire care spectrum that is utilizing a digital or IRL human counterpart to achieve better health outcomes. While physicians direct ~80% of all healthcare spend, an entire layer of subclinical human capital is emerging higher up in the care funnel to prevent patients from developing chronic conditions or to provide more accessible and trustworthy clinical care pathways to rising-risk and high-risk populations by solving social issues first.
In my last publication (from my personal newsletter), I briefly covered the success that fitness & wellness companies have seen from leveraging digital coaches to drive greater client adherence to prescribed fitness, wellness or nutritional plans. These include Future for personal training, Noom for nutrition, or Mighty Health for healthy aging.
Across the formative layers that aim to contain risk in health care utilization and cost, health behaviors such as exercise or diet are arguably the most manageable given that engagement is predicated on the ability to manipulate one’s own behavior.
For example, some people are fortunate enough to live in a world with little relative hardship in which they can actively choose to exercise, theoretically helping to reduce the total cost of care down the line if maintained. But adherence is tough given work/life schedules, various digital experiences increasingly vying for attention and the general lack of willpower. If you read that last sentence out loud a couple more times, you start to realize that most of today’s issues for the middle and upper class aren’t “real” issues, but more so desired lifestyle conflicts. As such, leveraging a human counterpart (e.g., digital coach) to drive better accountability is low hanging fruit given the variables that need attention are primarily in one’s control.
Other formative layers aren’t so easy. Individuals that reside in low-income communities often have to deal with factors out of their own singular control such as neighborhood and physical environment, socioeconomic conditions, transportation options, and education and employment accessibility. These ZIP code-based factors and the resulting health behaviors represent a community’s social determinants of health (SDoH). SDoH factors influence 80% of health outcomes and have expansionary effects on both the rising-risk population and racial health disparities if left unmanaged. For those affected, help from another human or a coordinated team is the only way that they can get out from under these repressive factors. However, designing social care pathways for this heterogeneous population is a much more difficult task, requiring a high degree of empathy and cultural competency.
Individuals within the older adult population also have their own set of uncontrollable factors such as the lack of universal design or the loss of a partner. As more attention is being called to manage these formative layers across Medicare and Medicaid populations, innovation that leverages a subclinical human counterpart is progressing beyond low-hanging, health behavior-based opportunities to take on more complex, accessibility-based ones.
The hidden heroes that buttress these new experiences not only are helping to affect upstream SDoH factors that will result in greater access to downstream health care, but also are helping to alleviate the healthcare labor shortage by shifting to more community-based care.
Let’s examine the current pain points within health care accessibility for high-risk and rising-risk populations under public coverage and analyze the various service models being deployed today.
Pain Points
👵 High-risk population
The high-risk population includes high-need, high-cost patients who make up only 5% of patients but account for ~50% of public healthcare spending.1 It shouldn’t come as a surprise that older patients are far more likely to be high-risk than younger ones given that ~85% of patients aged 65+ have at least one chronic disease and 60% suffer from comorbidities.2 As a result, older adults generate the highest health care spend per capita.
While most older adults are enrolled within Medicare Advantage (MA) or Original Medicare plans, getting to a physical doctor’s office can be difficult for those without family support or those with disabilities. Unfortunately, given a lower relative investment in healthy aging (e.g., physical activity), Americans spend nearly one-third of their post-65 years dealing with some form of disability. For comparison, this number in Japan is just 9%.3 Additionally, the increasing percentage of older adults preferring to “age in place” only exacerbates the logistical strain around health care accessibility.
Disabilities also make it hard for older adults to complete daily activities that ultimately prevent acute incidents or the development of additional chronic conditions. These activities include picking up medication, getting groceries or cultivating companionship with others, just to name a few.
📈 Rising-risk population
The rising-risk population is a growing blind spot for plans, totaling 25%+ of patients and consisting of emerging risk members who could become the high-risk members of tomorrow.
Elevated SDoH risk across low-income communities is a large contributor to the increased number of rising-risk patients within Medicaid, which plays a disproportionately large role in covering people of color.
Sadly, there is no disputing the longstanding racial and ethnic disparities in health care. Within the managed care programs that provide coverage to 70% of the total Medicaid population, studies have shown that underrepresented enrollees reported significantly worse health care access and experiences than white enrollees. Overall adjusted disparities for African American enrollees ranged between -1.5 and -4.5 percentage points; -1.6 and -3.9 percentage points for Hispanic or Latino enrollees; and -9.0 and -17.4 percentage points for Asian American, Native Hawaiian, or other Pacific Islander enrollees.4
This negative sentiment along with numerous historical, government-led atrocities (e.g., Tuskegee Experiment) trigger a contagion of mistrust in terms of how people of color perceive the healthcare system. Structural racism and the lack of both culturally competent services and patient-provider concordance combined with factors such as housing, food and transportation insecurity create a vicious care inhibiting cocktail that results in the health inequity we see today.
Human-led Solutions
The common thread across the high-risk and rising-risk populations is the fact that health care accessibility is predicated on formative, social layers that often require a human counterpart to manage. Let’s take a detailed look at a couple available solutions that are tackling the various aforementioned pain points.
Papa
Papa partners with MA plans nationwide to connect beneficiaries to young adults for help with doctor appointments, car rides, house tasks, medication pick up and companionship. The company has over 25,000 “Pals” (average age is mid-30s) that are trained on empathy, cultural competency, and humility.5 Think gig economy for assisting older adults in which the most dedicated Pals earn ~$3,000 per month!
The social-first, clinical-second service helps beneficiaries mitigate logistical strain and isolation as they live out their golden years. The latter aspect of eliminating loneliness through companionship is particularly important, helping to cultivate meaningful relationships that ultimately result in the most important factor of all - trust.
It’s trust that allows the Pals to eventually drive heightened beneficiary awareness around the importance of completing annual wellness exams, filling out personal health risk assessments and undergoing covered health screenings. The Pals’ ability to drive higher engagement rates for these actions not only provides Managed Care Organizations (MCOs) with trusted information that allows them to discover member health issues dynamically, but also helps to boost their plan Star Ratings, which are based on quality of care and customer service measures. Health plans that receive at least four stars qualify for bonus payments from Medicare.
Since 2020, more than 65 MA plans have signed up with Papa in which they pay a per member per month (pmpm) fee for each engaged beneficiary.6 With the fastest growing segment of older adults forecasted to be the “oldest-old” (i.e., 75+) who are disabled at the highest rates, Papa and its human-led approach stand to function as a meaningful partnership service for plans as they do everything they can to differentiate offerings and to contain health care spending going forward.
Lukan Group
We recently had an incredibly enlightening conversation with the Lukan Group, a faith-based service organization that is building trust networks to increase care accessibility within underrepresented communities.
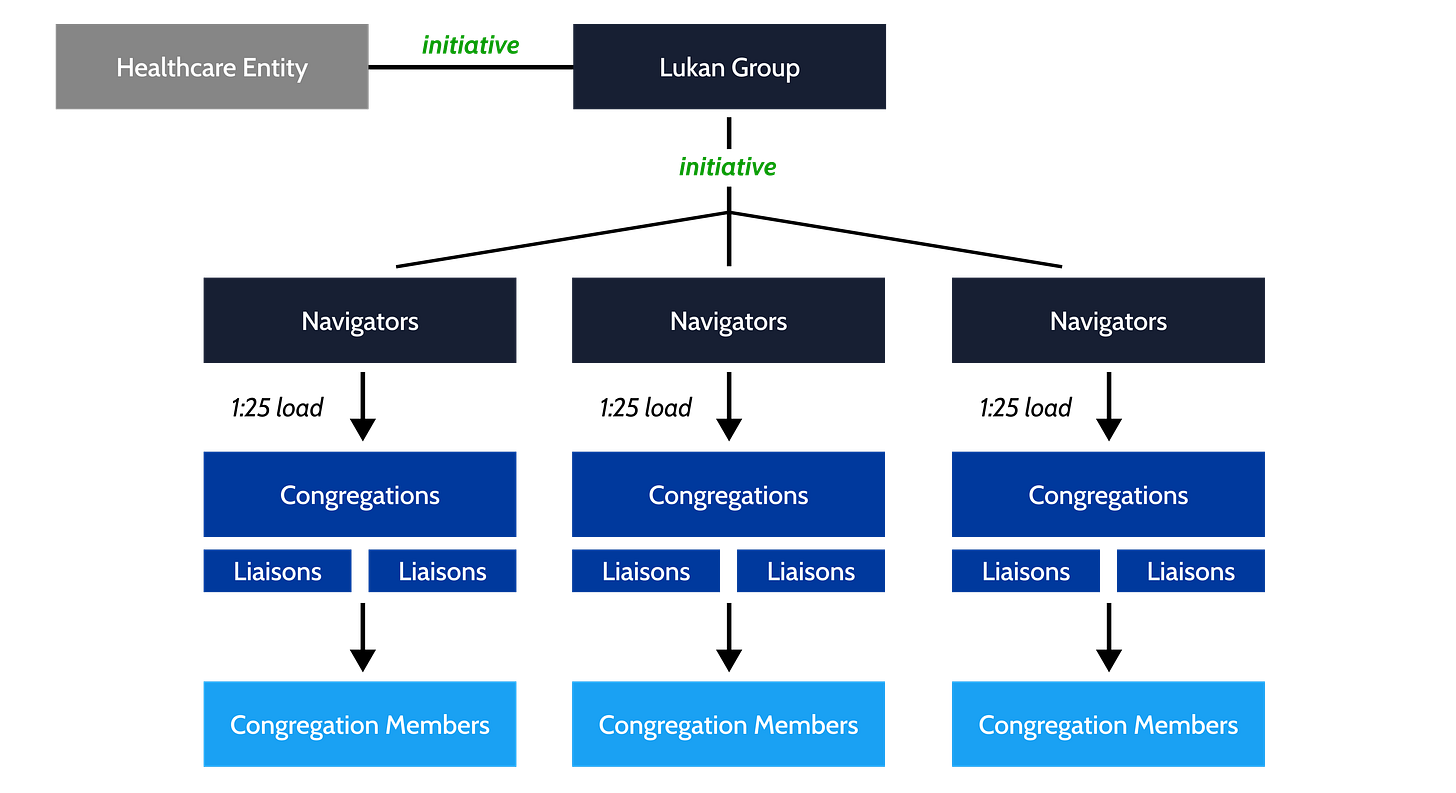
Led by former Centers for Medicare & Medicaid Services (CMS) executive Dr. Terris King, the organization functions as a health and wellness intermediary that leverages congregational trust to improve quality of care, reduce health care costs and eliminate disparities. Their human navigator-led model, which is being utilized in churches across 20 states, engages congregations as community health assets that partner with healthcare entities (e.g., payers, health systems, biopharma) to educate members and to improve health outcomes. The Lukan Group effectively gives healthcare entities gravitas in “hard to reach” communities, lending credibility to those that they partner with. Said another way, members of the communities that the Lukan Group serves do not trust a hospital system, but they trust their local congregation leaders.
The organization’s success is predicated on its navigators and their ability to direct traffic for partnering health entities. Each navigator supports ~25 different congregations, which have their own respective, trained liaisons that drive awareness and trust among their congregation members. For example, within the city of Memphis alone, Lukan Group navigators worked with 700 trained congregation liaisons (all volunteers) across more than 500 congregations. The total reach covered over 20,000 members that are now accessible through the Lukan Group network.
In order to establish trust within underrepresented communities that have historically mistrusted the healthcare system, Dr. King couldn’t stress the importance of two core factors enough - (1) community reinvestment and (2) messenger concordance.
🏘️ Community reinvestment
The Lukan Group first vets potential partnerships by listening and processing a healthcare entity’s understanding not only of how it will benefit clinically from accessing a community (e.g., increasing vaccination rates, access to underrepresented clinical trial enrollees), but also of how it will benefit individuals and the community at large. The importance of the latter cannot be overstated as community reinvestment is table stakes when it comes to establishing a bi-directional relationship with underrepresented communities. Healthcare entities need to come into communities and address neighborhood and sustainability aspects first before clinical messaging will ever be entertained.
Dr. King shared an evocative story in which a prospective partner was looking to access a particular community for the first time. After being educated on the importance of employing a “what do you need?” approach to start, the prospective partner was connected with relevant community leaders and members via the Lukan Group network. The community leaders and members begged the healthcare entity to help them figure out how to eradicate a rodent infestation that was affecting their youth playgrounds where children were often bitten and subsequently exposed to viral disease. And it wasn’t until the healthcare entity was able to provide ongoing resources to remedy this situation that the community was then willing to hear their health-related initiatives.
“People don’t care how much you know until they know how much you care”
- Dr. Terris King, CEO, Lukan Group
🫂 Messenger concordance
The proverbial “don’t kill the messenger” phrase is a real factor when it comes to the dissemination of clinical messaging within the communities that the Lukan Group serves. Trust is paramount for driving health care engagement, yet unattainable for healthcare entities looking to penetrate communities that they inherently misunderstand.
The only way that these healthcare entities can achieve cultural competency and messenger concordance is by partnering with service organizations like the Lukan Group who are deeply ingrained in the community through faith.
Story time again. This one is titled “Lady in the Window”. A home health agency recently reached out to congregational liaisons in hopes to gather more information on a member of their church. This member had repeatedly signed up for a home health screening. However, every time the agency showed up to her home for the scheduled appointment, no one would answer the door. It didn’t make any sense.
What the agency didn’t know was that this particular woman spends her days sitting in a room toward the back of her home. Anyone that the woman is familiar with and trusts knows that she sits in this room, in her favorite chair, next to a window. If you want her to come to the door, you knock on the window, and she will let you in. For this woman, access is determined by relationship, not an appointment. She knows that you know her because you came to the right window.
Within most underrepresented communities, the church knows things that hospitals and health services companies will never know. And without this community-based knowledge and earned trust, health care accessibility and education will perpetually be in a stalemate.
“They won't hear you because they don’t know you”
- Dr. Bobby Baker, President, Lukan Group
By growing their accessible network through navigators and liaisons, the Lukan Group effectively functions as a trellis that can grow anything intended to be in relationship with underrepresented communities. The organization’s focus on leveraging its influence to improve quality of care, reduce health care costs and eliminate disparities provides partners with the trust and messaging alignment that they could never realize themselves.
As more states add SDoH requirements to managed Medicaid contracts in effort to ameliorate health care inequity, the utilization of human-led service organizations like the Lukan Group and/or the growing number of human-led “tech + touch” services startups will become vital in order for MCOs to meet newly instituted performance measures. I will note that despite the endemic knowledge that organizations like the Lukan Group have been able to draw attention to, it’s surprising to see community reinvestment requirements with the least adoption across states.
In addition to payers, health systems and biopharma companies also have an increasing focus on improving health equity & SDoH. Below are some of the leading human-led, social-first companies and organizations that are helping these major healthcare stakeholders tackle this formidable challenge.
Final Thoughts
As more emphasis is placed on addressing formative layers of care for riskier populations, we should expect to see more social care pathways utilize human-led components such as advocates, navigators or caretakers to provide empathy, to garner trust and to ultimately provide better access to downstream health care. While population health studies have shown that solving upstream SDoH pain points can deliver causative reductions in total cost of care, execution at scale remains difficult, especially when engaging more heterogeneous populations within Medcaid that require meaningfully more touch and IRL intervention.
As a human optimization investor based in the most tech-forward city in the world, it’s easy to get excited by care solutions aimed at increasing longevity, maximizing performance or providing tech-heavy, concierge service models. While each of those use cases have extraordinary promise, not enough awareness is being driven outside of the captive privilege bubble and on innovation that can provide better care access to the large, yet often marginalized populations that need it most. While still in the early innings, the progress of human-centric, social-first solutions that are purpose built for CMS populations are inspiring and certainly prove that not all heroes wear capes (or white coats).
If you are building or investing within health & wellness, we’d love to chat! Please reach out to jordan@nextventures.com or head over to our website.
https://www.fiercehealthcare.com/practices/how-can-healthcare-improve-care-for-high-need-high-risk-patients-just-ask-them
https://www.nia.nih.gov/health/supporting-older-patients-chronic-conditions
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1464018/
https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2021.01331
https://www.washingtonpost.com/health/2022/03/12/medicare-advantage-athome-helpers/
https://www.washingtonpost.com/health/2022/03/12/medicare-advantage-athome-helpers/








Insightful and informative as always. Thanks for sharing the data & a few human-led solutions.
"Health care accessibility is predicated on formative, social layers that often require a human counterpart to manage."