Our 20th Investment: Pair Team
Enabling better health outcomes for our most vulnerable communities.
It’s been nearly two years since we launched our renewed thesis on whole-person health, expanding our focus across the upstream and downstream layers of care with an emphasis on opportunities that drive greater access and health equity.
Since that pivotal moment, we’ve been fortunate enough to partner with some exceptional teams that are driving innovation across point-of-care diagnostics, primary care, behavioral health and clinical trials enrollment, just to name a few. The collective efforts of our portfolio companies have touched millions of lives, and we’re incredibly humbled by this feat. That being said, innovation within one population of focus in particular has stayed top of mind for us - Medicaid.
We couldn’t be more thrilled to partner with Neil, Cassie and Pair Team as they continue their mission of connecting underserved communities to high-quality care and driving innovation within Medicaid managed care. Our relationship with Neil and Cassie traces back to this time last year, and we’d love to pull back the curtain on how this exciting partnership came to be.
Background
We’ve spent the last year and a half in a deep learning state as it relates to understanding the unique care model elements needed to succeed in Medicaid managed care. This consisted of a bottoms-up approach that started with community.
The first step was making a deliberate effort to connect with the leaders of community support organizations in low-income communities. These crucial stakeholders emphasized the importance of community reinvestment and messenger concordance before disseminating any type of clinical messaging. Based on this feedback, it was abundantly clear that initial engagements with the Medicaid population must be focused on earning trust and solving SDoH-related issues. They also shared intimate stories from their respective communities that further substantiated this point. For those who’ve kept up with our newsletter, this includes the evocative “Lady in the Window” story from our Hidden Heroes of Healthcare post. If you haven’t checked it out already, it’s worth a read here!
The next step was to align with key opinion leaders and operators who have driven progress and innovation within Medicaid from a payer, provider and/or regulatory perspective. This resulted in the appointment of R.J. Briscione to our Advisory Board last year to help us keep a pulse on Medicaid developments and to serve as an asset to our current and future founders serving this population. R.J.’s experience spans over a decade long, championing and leading SDoH Strategy at CVS Health, leading Medicaid Business Development for Aetna’s East Region, and serving as director of Medicaid and Duals operations in multiple states for Anthem. R.J. also serves as an advisory board member for the Medicaid Innovation Collaborative, which aims to improve the health and wellbeing of individuals on Medicaid through tech-enabled innovations.
With these two pieces in hand, we dove into the ecosystem of Medicaid managed care, spending time with fearless founders building in the space and taking note of upmarket success around the enablement of accountable care models in adjacent at-risk populations such as Medicare.
In terms of the latter point, we’ve grown increasingly encouraged by the overall progress within VBC enablement across both public and private markets and we believe that there’s an interesting opportunity for VBC enablers to grow beyond Medicare as they look to capture a greater share of partnering providers’ panels (full thesis here). That said, Medicaid and commercial inherently have lower alternative payment model (APM) uptake today versus Medicare, which is not surprising given the relative lack of built-in risk adjustment opportunities and the lack of established accountable care models (e.g., ACO Reach, KCC) to build on top of.
When R.J. introduced us to Neil and Cassie in the Fall of last year, it was as if the stars aligned, bringing together our interest in Medicaid and VBC enablement through one opportunity. Not to mention being led by two passionate founders with strong experience building and delivering cutting-edge care models.
Not only is Pair Team enabling better health outcomes for our most vulnerable communities through a social-first, clinical-second model of care, but they’re also doing so through an approach that’s built on top of the contracting and payment rails of California’s Enhanced Care Management (ECM) model, and CalAIM more broadly.
ECM addresses the clinical and non-clinical needs of the highest-need Medicaid members by building trusting relationships with members and providing comprehensive care management and intensive coordination of health and health-related services.
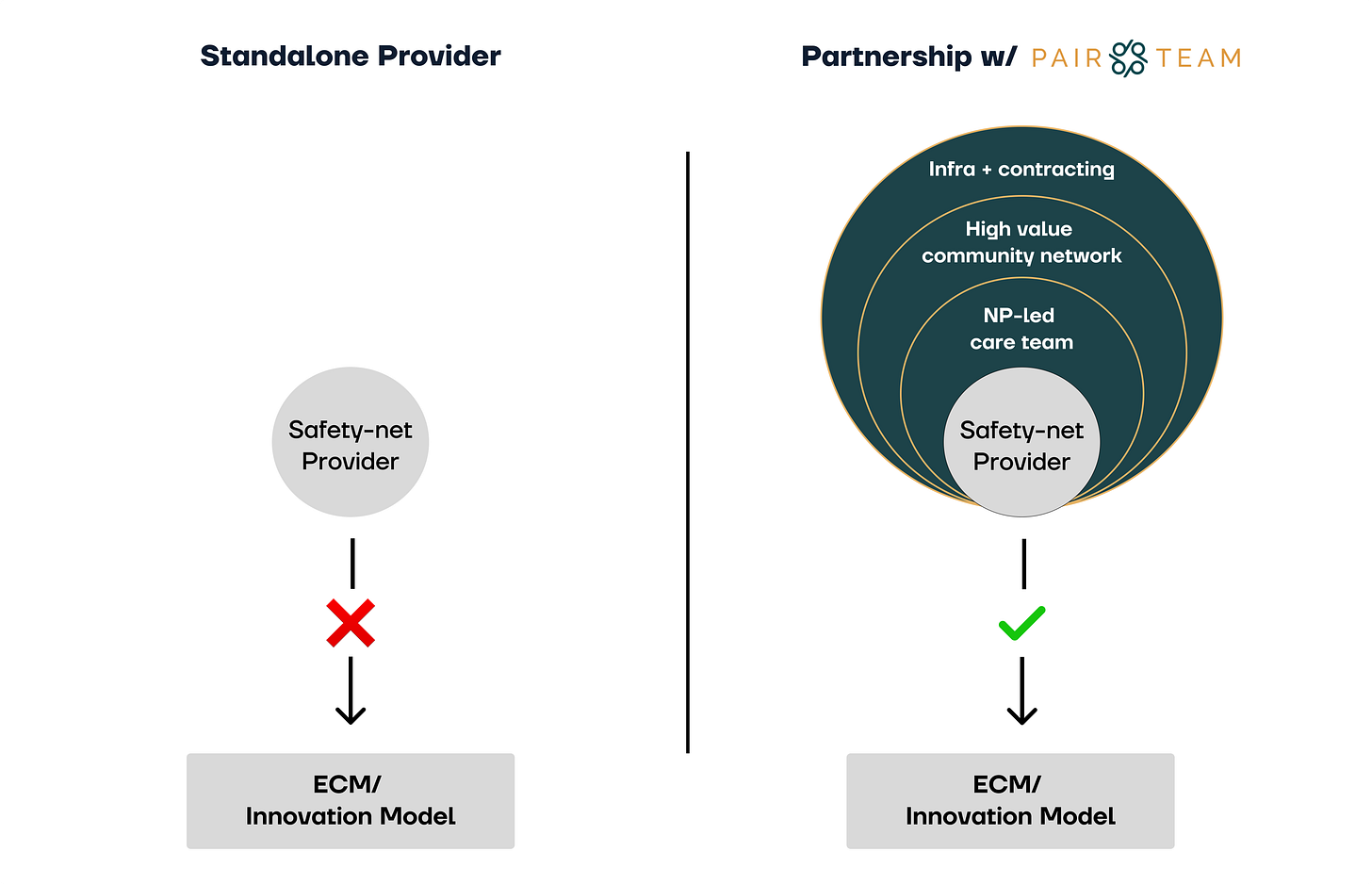
The launch of ECM represented a milestone for Medicaid managed care in California and serves as a leading precedent nationally. And yet, the severely under-resourced nature of local clinics and community-based organizations (CBOs) who provide care to the vast majority of the Medicaid population creates a chasm in the model design, precluding those providers from enrolling high-needs lives into ECM in the first place or from providing the ongoing care management required under model stipulations.
In classic VBC enablement fashion, Pair Team addresses this chasm by partnering with local clinics and CBOs and providing them with the wraparound products and services needed to successfully participate in ECM. These include an NP-led multi-specialty team, a network of safety net organizations, tech infrastructure, and ECM contracting.
This changes the lives of the 600,000+ high-needs Medi-Cal members (and the 15M total Medi-Cal members more broadly) who’ve historically struggled to access the care needed to better their health. Pair Team’s virtual and community-based solution builds personal and meaningful relationships with patients to help them regain trust in and access to the health care system, bringing whole-person care to more patients right here in our backyard, and soon in other states.
While the team’s progress across enrollments, engagement and improved health outcomes has been stellar, the most promising observation over the past year has been the heartfelt feedback from patients who speak to the role Pair plays in their lives. Pair serves as a beacon of hope and an unwavering shoulder to lean on for those in our most vulnerable communities and we couldn’t be more humbled to have the opportunity to drive their mission forward.
We are joined by the California Health Care Foundation, OCA Ventures, Kapor Capital, Create Health Ventures and other add-value investors who share the vision of driving better access to whole-person care for high-needs Medicaid members.
Every month we write a piece encompassing themes within our whole-person health investment thesis. If you would like to receive it directly in your inbox, subscribe now.